Sunday, December 25, 2022
Sunday, December 18, 2022
Bluetooth Physiotherapists?
The aim of the published article was to assess how 125 physiotherapists assess muscle stiffness on a 7-point palpation scale generated by a novel device. Measurements of displacement, force and stiffness were recorded.
Physiotherapists always use their hands to palpate muscle tension (or muscle tone), which is commonly known as muscle stiffness, among other assessments. It is then standard practice to base some subsequent treatment on these palpation findings. Of course these assessments can be considered subjective and may vary from one physiotherapist to another. It's accuracy and repeatability will depend on each physiotherapist's skill and experience.
At the same time, there are heated calls within the Physiotherapy profession to stop hands-on manual therapy (or passive physiotherapy treatment) since it creates dependence, low value in care and is not totally evidenced based. Physiotherapists who work in hospitals here in Singapore and elsewhere have practically eliminated this form of 'passive' treatment when treating patients. Physiotherapists who support these views are affectionately called 'bluetooth' (or hands free) physios.
Would a 'bluetooth' physio be able to palpate accurately and consistently compared to another physiotherapist who only uses their hands for assessing and treating? That is probably why the above mentioned research paper concluded that palpation is 'not reliable' to diagnose pathology and develop treatment protocols.
While the physiotherapy community argues whether we should or should not be using hands on manual therapy, the massage therapy, chiropractic, osteopathy, personal training and strength and conditioning professions will be watching us fight online, waiting to take over our patients while we complain that they are practising certain treatments 'beyond' their scope.
Do not complain if you don't want to do it, but just be aware others will. Remember when physiotherapists used to complain about doctors who don't even bother to examine their patients?
If you are a 'bluetooth' physiotherapist and do not want to use your hands to treat your patients, do not criticize another physiotherapist who does it appropriately. Perhaps consider asking yourself what your patients want and need. Patients will vote with their dollars and seek alternative treatment, if their physiotherapist isn't able to solve their problem.
Of course, even perfect palpation skills on it's own may not be enough, since muscle stiffness is just one aspect of the assessment. You have to put together history, mechanism of injury, interpret movement direction, symptom provocation etc to decide treatment selection for your patient. The muscles you are palpating may not even be the cause of the problem even though it is 'stiff'.
Reference
Davidson MJ, Nielsen PMF, Taberner AJ et al (2019). Is It Time To Rethink Using Digital Palpation For Assessment Of Muscle Stiffness? Neurourology and Urodynamics. 39(1): 279-285. DOI: 10.1002/nau.24192
.png) |
| From Tiktok |
Sunday, December 11, 2022
Can You Get Sicker If You Exercise With A Cold?
Being a die-hard exercise devotee, there was no way I was going to miss my exercise session. Was that the right decision? Does that mean if you have a runny nose you need to skip your exercise session or could that workout actually do you some good?
In the past, I've always gone by the 'neck' rule. Symptoms above the neck (like a runny nose or low grade headache) means that a light workout usually will not make your cold or ailment worse.
The 'neck' rule was based on research done by Dr Weidner and colleagues. 50 adults that were infected with the common cold virus were randomly split into 2 groups. One group (34 subjects) had subjects do 40 minutes of moderate exercise every other day for 10 days while the other group (16 subjects) did no exercise.
The researchers found no difference in illness length or severity between the 2 groups. This shows that exercising moderately did not prolong or exacerbate their illness.
However, if you have below the neck symptoms like a hacking cough, chest discomfort, nausea, diarrhoea or whole body symptoms like fever, muscle aches or fatigue then it's not a good idea to exercise.
Please bear in mind that symptoms can evolve and what started as a runny nose can worsen to something more serious like the flu or even bronchitis. If your symptoms get worse, it's probably best to have a rest day. Rest till the 'below neck' symtoms go away. Relapse can happen if you try to come back too quickly and push too hard.
In rare cases, exercising intensely when you are sick or shortly after you have recovered can lead to new or lingering symptoms like exhaustion or unexplained pain. Researchers believe this is similar to how people develop long Covid or chronic fatigue syndrome.
If you are a die-hard exercise fanatic, try a brisk 30 minute walk outside or get on the stationary bike or elliptical machine. Lifting weights, like what I did, is probably fine too, just don't attempt to beat your personal best lifts. You will probably feel a psychological boost after exercising if all goes well.
Call it quits if you feel light headed or develop chest tightness or feel too much pain. Ease back slowly to your exercise routine when you're fully recovered before gradually increasing duration and intensity. Research actually shows that moderate exercise even when you're healthy helps to improve your immune response and lower your risk of catching respiratory tract infections.
References
Pedersen BK and Toft AD. (2000). Effects Of Exercise On Lymphocytes And Cytokines. BJSM. 34: 246-241. DOI: 10.1136/bjsm.34.4.246
Weidner TG, Cranston T, Schurr T et al (1998). The Effect Of Exercise Training on The Severity And Duration of A Viral Upper Respiratory Illness. Med Sci Sp Ex. 30(11): 1578-83. DOI: 10.1016/S0765-1597(99)80059-8
Wednesday, December 7, 2022
We Went Batik Painting
Kamal actually apologized for telling us all that. But being interested in history, I was impressed by his passion and knowledge. I told him hat it was good he shared that.
 |
| Tools of the trade |
 |
| The wax |
Here's us at the exhibition center.
Saturday, December 3, 2022
Shift Work And Pain
Shift work means businesses and organizations can be productive 24 hours a day. With the development of artificial lighting, manufacturing, service and retail sectors have used shift work to increase productivity and profitability. It also allows for the provision of continous healthcare and emergency services.
I found out that the Cold Storage in Holland Village across the road from our clinic pays a monthly rent that is in excess of $200,000 a month. That's probably one of the reasons why they are open 24 hours. To maximise what they already pay for rental.
So I was not surprised to read that shift work, in particular night work is associated with chronic musculoskeletal pain (Matre et al, 2021). The mentioned study had 23,223 subjects which was adjusted for sex, age and education reviewed significant associations between shift work and chronic musculoskeletal pain and chronic pain sites.
It is estimated that 20 percent of the workforce are now shift workers, with 25 to 30 percent of those working nights.
Evidence now shows that working when you're supposed to sleep and rest disrupts your normal physiology. Growing evidence points to the disruption of the circadian clock caused by being awake or active at nigt when we're supposed to sleep.
All living species since evolution, from bacteria, plants to animals have acquired a circadian clock to optimize body processes in an environment that changes throughout the day. We are rhythmically organized to anticipate these daily changes.
Our immune system, muscular system and cognitive performances are higher in the day when the body is also storing nutrients from food. The functions decrease at night when the body starts to use he stored nutrients during this period of fasting.
Just like a conductor of an orchestra, our central clock in the brain synchronises all the circadian clocks along with environmental light. If these clocks get input from other sources like food or other light sources at night, this synchrony is lost.
Shift work simulation has been shown to affect the immune system. This contributes a higher risk of infection among shift workers, notably Covid-19.
Circadian disruption is also associated with disturbance of our the autonomous nervous system which controls breathing and our heart beat. This affects the connection between the brain and its surrounding tissues and their proper function.
This contributes globally to weight gain, Type II diabetes, increased blood pressure, compromised immune response and chronic musculoskeletal pain. This lost synchronicity also leads to a increased incidence of breast cancer, faster tumour growth and also exacerbates Alzheimer's disease. This is seen even in cases of low intensity light in the bedroom coming from a TV screen.
What can we do about it? The first step should be to limit rotating shift work as much as possible. It is somewhat possible to adapt to work at the "wrong" time but impossible to adapt to schedules that constantly change.
Some studies showed that bright light increases alertness during the night and helps adaptation to night work by shifting the circadian clock. However, long term impact on health is still unknown.
Controlling and limiting the time during which we eat (e.g. 10 hours during the day and not eating overnight) appears to be beneficial for heart and metabolic health (Sutton et al, 2018). This may be compatible with shift work.
There is probably no optimal solution for this unless we limit shift work to just essential hospital services. This may then help reverse the global trend towards a 24 hour society to decrease shift work for better health.
Are we able to take that huge step? Especially when most countries are opening up again after Covid-19.
References
Dun A, Zhao X, Jin X et al (2020). Association Between Night-shift Work And Cancer Risk: Updated Sysyematic Review And Meta-analysis. Front Oncol. 10:1580. DOI: 10.3389/fonc.2020.010006
Manouchehri E, Taghipour A, Ghavami V et al (2021). Might-shift Work Duration And Breast Cancer Risk: An Updated Systematic Review And Meta-analysis. BMC Women's Health. 21: 8. DOI: 10.1186/s12905-021-01233-4
Matre D, Christensen JO, Mork PJ (2021). Shift Work, Inflammation And Musculoskeletal Pain -The Hunt Study. Occu Med (Lond). 71(9): 422-427. DOI: 10.1093/occmed/kqab133.
Sutton EF, Beyi R, Early KS (2018). Early Time-restricted Feeding Improves Insulin Sensitivity, Blood Pressure, And Oxidative Stress Even Without Weight Loss In Men With Prediabetes. Cell Metab. 27(8): 1212-1221. DOI: 10.1016/j.cmet.2018.04.0
Sunday, November 27, 2022
Will Marathon Running Hurt Your Back?
 |
| Spot my compression fracture at L1? |
 |
| My L1 is 'collapsed' compared to above and below |
Sunday, November 20, 2022
Is Yoga Helpful For Low Back Pain?
This latest Cochrane review that was just published 2 days ago, evaluated whether yoga was beneficial or harmful for treatment of non specific low back pain. Review articles from the Cochrane Database of Systematic Reviews are highly respected and trusted.
The review wanted to find out if yoga helps improve function (getting dressed, walking or housework), quality of life and pain associated with low back pain. Medical databases searched for randomized controlled trials of yoga compared to sham (fake) yoga, no treatment, any other treatment and yoga added to other treatment.
Altogether 21 trials with 2223 participants (mostly women in their 40's or 50's) were found. 10 trials from USA, 5 from India, 2 form UK and 1 each from Crotia, Germany, Sweden and Turkey.
10 studies compared yoga to no exercise control group which received usual education and were put on a waiting list for yoga. 6 studies compared yoga to back-focused exercise or similar core exercise programs. 5 studies compared yoga, no exercise and qigong.
At 3 months, there was low to moderate evidence that yoga was slightly better than no exercise in improving back function and pain, although the difference were not sufficiently important to the person with low back pain.
There was low quality evidence for better clinical improvement with yoga while there was moderate quality evidence for a slight improvement in both physical (able to be active) and mental (emotional problems) quality of life. Evidence was of very low quality for helping depression. In addition there was moderate quality evidence that there was little or no difference between yoga and other types of exercise in improving back function and pain.
Increased low back pain was the most commonly reported 'harmful' reaction and there were no reported cases of serious side effects. There was low quality evidence that the risk of harm was higher with yoga than no exercise and back-focused exercise.
No studies comparing yoga to sham yoga were found, so there is no evidence how yoga would affect low back pain if people did not know they were doing yoga. All the participants knew they were doing yoga and this may influence their interpretation of whether their back pain has changed.
There you have it, quite different from what you have been told, heard or read. Our goal is to help patients confidently take up different movement, postures, physical activity, social and work engagement so you can can a healthy and pain free life.
There are free educational resources to support these processes if you do have low back pain and have not seen us in our clinics.
You can watch this Youtube video or visit this site for more details. This will help reduce stress and build self sufficiency for you to better self manage your LBP and make better informed choices about your care.
Our spine is strong, robust and adaptable. A campaign to change this may encounter resistance even in the physiotherapy and ergonomic professions as their business model may not be in line with what we now know to be best practice for managing low back pain.
So here's my take, whether it's yoga, pilates, stationary cycling or any exercise, it is your choice, as long as you keep doing it consistently, it will help your low back pain. Find an exercise you enjoy and keep at it.
Reference
Wieland LS, Skoetz N, Pilkington K et al (2022). Yoga For Chronic Non-specific Low Back Pain. Cochrane Database of Systematic Reviews. Issue 11. Art. No : CD010671. DOI: 10.1002/1465.CD010671
Sunday, November 13, 2022
Should You Be Taking Creatine?
Creatine use back in the 90's was popular because it actually did what was claimed on the container (unlike many other supplements). It definitely changed how sports nutrition was viewed.
Creatine is a natural compound in our body produced from amino acids. It is also found in red meat and some fish. In our muscles, it is called phosphocreatine (or free creatine) where it is necessary for enabling movement and exercise. Phosphocreatine is responsible for quickly restoring ATP levels in muscles, which functions as the 'energy currency' for cells.
ATP is broken down (or used) when our muscles contract during exercise and other activities. Phosphocreatine provides a qiuck pool of energy to allow quick restoration of ATP, which is fuel especially for high intensity exercise. Since creatine exist only in small amounts in the body, it is enough to fuel about 10 seconds of intense effort or all out sprint. Hence this is the 'free creatine' energy we all have in our bodies when needed for that 10 seconds worth of intense exercise.
Note that the body can also produce ATP from carbohydrates and fat, but it is a relatively slow process.
How creatine works is that it is able to produce strength gains because it enhances the short term, high intensity energy pathway in muscles called the phospho-creatine (PC) system.
If the PC system is enhanced, it allows our muscle fibers to contract vigorously for longer periods allowing more intense loading and fatigue for the muscles. After the muscles break down, it produces greater repair and growth stimulus with adequate rest and nutrition This ultimately results in greater strength gains.
Taking creatine supplements can increase creatine stores in the body by up to 30 percent. Many types of creatine are available, the cheapest and most researched being creatine monohydrate. Bear in mind that the pricier creatine hydrochloride and ethyl ester have not been proven to be superior.
Many people who take creatine start with a loading phase of 20-30 grams per day (for up to 7 days) to saturate stores quickly, leading to a rapid increase in muscle stores of creatine. Subsequently, they take 3-5 grams daily to maintain levels.
Those who choose not to load will consume 3-5 grams daily. Research shows this is just as effective and it will take up to a month to maximise stores this way before it has an effect.
A known side effect of consuming creatine is weight gain since creatine causes water retention in your muscles. This weight gain varies between 1-3 kg and not everyone who takes creatine experiences it. It can also cause mild stomach discomfort when large doses are taken. Long term supplementation with high doses have been investigated and shown to be safe in healthy subjects (Kreider et al, 2017).
Creatine supplementation is extremely popular with sprinters, strength and power athletes, especially when their events last for less than 30 seconds. It increases muscle mass and strength during weight training as well as improving performance during competition.
Since body weight is not as important in sprints, weight and power lifting, athletes from these sports can benefit as increases in performance more than compensates for the increase in body weight.
Those who participate in sports like soccer, basketball or hockey when intermittent short bursts of high intensity sprints and jumps are required will benefit with creatine supplementation. Specific tests where power output and speed are improved have been shown in athletes in such sports (Ramirez- Campillo et al, 2016).
What about endurance sports? In ultra events, the need for high intensity surges or bursts are less frequent, so as exercise duration increases, benefits of creatine reduces. Research on endurance sports are mixed though most show no benefit. An increase in body weight from consuming creatine may increase energy requirements and require greater power output.
I was asked why I took creatine supplements since research does not show much support when I used to race triathlons. I mainly raced the Olympic distance (1.5km swim, 40km bike, 10 km run) triathlons where fellow competitiors may surge on the climbs during the bike or run section to breakaway or get a gap. As such, we do need to respond to such high intensity surges otherwise the race may be over if you get dropped.
This was the main reason I thought taking creatine may help, since I needed to be able to sprint intermittently during my event, especially up slopes or near the end of a race. Studies that investigate cycling using stationary bikes where slight increases in body weight may not affect performances show benefits from taking creatine. This may occur in similar scenarios that I mentioned in a climb during a race or a sprint finish where there is a need for higher power output or speed (Murphy et al, 2005).
At these times, phosphocreatine contribute heaps to energy production, so an increase in creatine stores may be helpful. Bear in mind that the increase in body weight that sometime accompanies creatine supplementation is sufficient to cancel out the benefits. Especially in a hilly or longer race.
Utimately I stopped taking creatine supplements after 3 months because I did put on 1-2 kg of body weight. In addition I was not sure if it helped my ability to sprint and close gaps. I naturally have a good amount of Type IIa and IIb fast twitch muscle fibers already so the weight gain was not justified.
If you, like my patients, have heard good results about creatine and want to try it, bear in mind the scenarios that I mentioned.
References
Kreider B, Kalman DS, Antonio J (2017). International Society Of Sports Nutrition Position Stand: Safety And Efficacy Of Creatine Supplementation In Exercise, Sport, And Medicine. J Int Soc Sp Nutr. 14:18. DOI: 10.1186/s12970-017-0173-z
Murphy AJ, Watsford ML, Coutts AJ et al (2005). Effects Of Creatine Supplementation On Aerobic Power And Cardiovascular Structure And Function. J Sci Med Sp. 8(3): 305-313. DOI: 10.1016/s1440-2440(05)80041-6.
Ramirez-Campillo R, Gonzalez-Jurado R, Martinez C et al (2016). Effects Of Plyometric Training And Creatine Supplementation On Maximal-intensity Exercise And Endurance In Female Soccer Players. J Sp Med Sci. 19(8): 682-687. DOI: 10.1016/j.jsams.2015.005. DOI: 10.1016/j.jsams.2015.10.005
Sunday, November 6, 2022
Only Some Runners Ran Faster Using Carbon Plated Shoes
 |
| Alphafly (L) and Vaporfly from weartesters.com |
Now that these super shoes are more easily available (since many other brands other than Nike also make carbon plated shoes), is it worth splurging on them? Especially if you're trying to clock a personal best timing in your next race.
How does the original Nike super shoe (the Vaporfly) work? There are 2 novel components to this question. First, the super thick cushioned midsole Nike calls ZoomX. This new foam is super light, 31 millimeters high at the heel, which is 50 percent thicker than comparable shoes without being heavier. You can squish it and it springs back to shape quickly. This means it returns all the energy you applied to squish it.Next is the curved carbon fiber plate inside the midsole (pictured above). It is thought that the carbon fiber plate(s) acts like a spring, bending as your foot lands and then catapulting you forward as it springs back into position. This helps running economy (reduces energy expenditure) so you can run faster.
Ever since Nike launched their Vaporfly in 2017, which has since been updated a few times, there have been calls and debates to have the shoe disallowed in competition. Opposers have labelled the shoe as technical 'doping'. When subsequent studies showed that these Nike shoes gave up to a 4 percent advantage (Barnes and Kilding, 2019), other runners were obviously upset.
Especially after two Nike sponsored runners in the United States used the prototype version at the 2016 Olympic trials (women's 1st and 3rd places) and qualified for the Olympics.
Shalaya Kipp felt that the prototype Vaporfly's kept her training partner, Kara Goucher (4th place), off the Olympic team after signing up with Skechers. She left Nike in 2014 beacause of the infamous Alberto Salazar "Oregon project". Had Goucher stayed with Nike, she may have qualified for her third Olympics in 2016. At the actual 2016 Olympics, the top 3 male finishers all wore the same Nike prototype shoe.
In fact Nike scored a major coup when they offered all other runners who qualified in the 2020 USA marathon Olympic trials a pair of the Alphafly's to level the playing field.
Before you buy a pair of carbon plated shoes, consider the following study. It was published just last month looking at 96 runners using 2 different prototypes of carbon plated shoes. The shoes differed only by the forefoot bending stiffness. The runners were first assessed for their VO2 max and maximum aerobic speed. Running economy and stride kinematics were also recorded during the trials.
The researchers did not find any significant difference in running economy between the 2 different shoe stiffness for the group as a whole. Some runners' running economy improved when the carbon fiber plate was stiffer while in other runners, their running economy deteriorated. To be more specific, the faster runners took advantage of the increased stiffness (carbon fiber plates) while the slower runners did not.
The authors emphasized the importance of individual response to using carbon fiber plates to enhance running performance is runner specific.
For now, the carbon plates remain street legal for us mortal runners in competition. If you do get them, remember to break them in with a few runs instead of just saving them for race day. The midsole thickness definitely makes your foot more unstable especially when going around sharp corners or while making a u-turn in an out and back route.
References
BarnesKR and Kilding AE(2019). A Randomized Crossover Study Investigating The Running Economy Of Highly-Trained Male And Female Distance Runners In Marathon Racing Shoes Versus Track Spikes. Sports Med. 49(2): 331-342. DOI: 10.1007/s40279-018-1012-3.
Beck ON, Golyski PR and Sawiki GS (2020). Adder Carbon Fiber To Shoe Soles May Not Improve Running Economy: A Muscle-level Explanation. Sci Rep. 10: 17154. DOI: 10.1038/s41598-020-74097-7
Chollet M, Michlet S, Horvais N et al (2022). Individual Physiological Responses To Changes In Shoe Bending Stiffness: A Cluster Analysis Study On 96 Runners. Eur J Appl Physiol. DOI: 10.1007/s00421-022-05060-9
Sunday, October 30, 2022
Is It Really Your Piriformis?
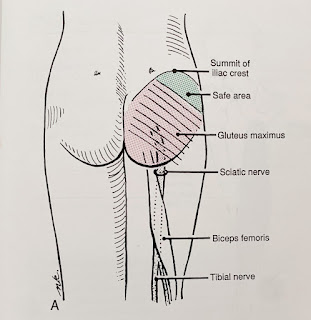
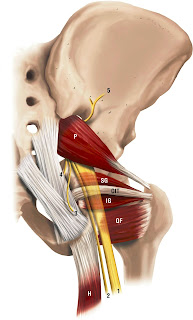
 |
| Right Piriformis muscle and the sciatic nerve |
The sciatic nerve can get encroached or irritated by the piriformis and adjacent structures in that deep gluteal space which may result in pain at the area of irritation or along the path of the sciatic nerve - this is true sciatica pain.
After assessing my patient, there was no pain nor tenderness in her piriformis. Instead, her obturator internus reproduced her buttock pain.Coincidently, I was fortunate to have read a recently published article exploring the relationship of the sciatic nerve and the deep hip external rotator muscles in the deep gluteal space (Balius et al 2022).
The authors recruited 58 healthy volunteers, 30 males and 28 females with an average age of 20.4 years plus or minus 7 years using real time ultrasound to quantify nerve action.
The sciatic nerve was found to be compressed (and moved forward and laterally) during passive hip internal rotation and isometric external rotation contraction (obturator internus and gemelli muscles working). Not the piriformis muscle, which the authors wrote were often over diagnosed.
During passive hip external rotation and isometric contraction of internal hip rotators, the sciatic nerve moved back into place and medially.
The obturator internal-gemellus syndrome may be a more accurate term than piriformis syndrome for my patient.
Interestingly, the same lead author, Balius and colleagues, published an earlier article in 2018 where they studied 6 fresh cadavers and 31 healthy volunteers. This study revealed the presence of connective tissue (or fascia) attaching the sciatic nerve to the obturator internus-gemellus tendons. The sciatic nerve was also affected similarly in the cadavers and subjects during passive hip internal rotation.
This newer study (Balius et al, 2022) provides further evidence that stretch or contraction of the obturator internus-gemellei complex will create some compression of the sciatic nerve at this level in the deep gluteal space. Definitely worth considering for those with buttock pain and sciatica.
The next time you have buttock pain or sciatica and the health practitioner treating you tells you that you have piriformis syndrome you may suggest it's not always the piriformis ;)
Reference
Balius R, Pujol M, Perez-Cuenca D et al (2022). Sciatic Nerve Movements In the Deep Gluteal Space During Hip Rotations Manuevers. Clinical Anatomy. 35(4): 482-491. DOI: 10.1002/ca.23828
Balius R, Sussin A, Morros C et al (2018). Gamellei-obturator Complex In the Deep Gluteal Space: An Anatomic And Dynamic Study. Skeletal Radiol. 47: 763-770. DOI: 10.1007/s00256-017-2831-2
Monday, October 24, 2022
The Big Picture
My main questions were, "How can I make myself better as a physiotherapist?", "How can I ensure that all the physios in my team get better?", "How can I make our clinics better for our patients?"
My thoughts were that I always have to keep up with the research that's out there, the solid ones of course. I keep my mind open to new ways of reading the human body and what is "normal". I look out for courses to upgrade my skills. These answers were just some of ones that came to mind.
I will of course be consulting with Aized and other colleagues for their thoughts of my questions. I'm curious to hear how they would answer my many questions. That's why I value my team. We see the world through different lenses, so I learn from their views too.
A very important group of people to consult too would be our patients. I want to find out what they think about their experiences at our clinics, and act upon them wherever needed.
This journey of life, of being a physiotherapist, of running our clinics is full of ups and downs. I keep my eyes on the big picture. The big picture is that each and every person who comes to our clinics feel heard, helped, understood and hopeful. That's really at the centre of all we do.
Sunday, October 16, 2022
My Patient Was Asked To Go For Functional Training
She was also told that that FT would improve her neuromuscular adaptations (increasing the efficiency the way her body moves and safety during activities related to daily living, work and sports). Other terms include high intensity functional training (HIFT) and functional fitness (FF).
I shared with her what I read regarding a review on whether FT programs are different from traditional strength, power, flexibility and endurance training programs that are already being used in the physical training of professional, recreational athletes, healthy adults and geriatric populations.
The authors focused on the FT definitions, exercises employed and the neuromuscular adaptations reported. Firstly, they found that there is no agreement on a universal definition for FT.
FT programs hope to improve the same neuromuscular adaptations similar to traditional strength, power and endurance training programs. The exercises employed are in fact the same.
The main confusion with these 'new' training programs is that (other than the new fancy names) they often always overlap with traditional strength, power, endurance and flexibility programs. There is also no precise definition of functional movements. Do our muscles perform any non functional functions?
Some studies have classified that FT involves resistance training while FF has been defined as a trend using strength training. So, both FT and FF can be easily described as strength training programs.
HIFT was defined as high intensity and high volume exercises with short rest intervals. This is similar to a strength, power, and endurance session elite athletes use during specific phases of training. In fact FF has also been known as HIFT. So FF is actually HIFT. Since exercise intensity is a training variable and not an exercise type, FT and HIFT is the same training program performed at different intensities.
The authors concluded that FT has no consistent and universal definition. FT programs and exercises are not different from those already used in sports training since the neuromuscular adaptations are the same. The authors concluded that FT is not different from traditional strength, power and aerobic endurance training.
In short, there is no "non-functional" or "traditional" training. There is no real need or rationale in classifying exercise training programs as FT.
The names of these new training progams may sound cool and fancy, but you now know that they are in fact similar to weight training.
The authors also recommended that the terms FT, HIFT and FF no longer be used to describe any training program. These can be easily classified as strength, power, endurance and flexibility programs. I found that a little too harsh since they are just names to describe training programs. At least now you know.
Reference
Ide BN, Silvatti AP, Marocolo M et al (2022). IS There Any Non-functional Training? A Conceptual Review. Frontiers Sport Active Living.3: 803366. DOI: 10.3389/fspor.2021.803366.
Sunday, October 9, 2022
Thoracic Outlet Syndrome
 |
| picture from mountainhp |
 |
| picture from J Manip Phy Therapeutics |
Individuals with compartment syndrome will usually complain of pain, paraesthesia (or pins and needles), their limbs (usually legs) being very tight, tense and full of pressure during training or doing the offending activity. Temporary paralysis can occur sometimes. It usually happens to athletes at the start of the season, after their break when they train too hard, too soon.
During exertion, the muscles expand and they fill up the space in the legs and "squeeze" the nerves and blood vessels there leading to sensations of tightness, pressure or pins & needles as the connective tissue that separates each section or compartment does not stretch hence leading to the term.
My patient probably has thoracic outlet syndrome (TOS) instead of compartment syndrome. TOS occurs when blood vessels or nerves in the space between the collar bone and first rib (this space is known as the thoracic outlet) are compressed causing neck, shoulder and arm pain and numbness in the arms and fingers.
There are a few types of TOS. My patient probably has the most common version known as neurological TOS, when the brachial plexus is compressed. The brachial plexus is a big network of nerves from the spinal cord and it controls muscle movements in the shoulder, arm and hand.
A common area where TOS occurs is in the interscalene triangle (formed by the brachial plexus, the subclavian artery exiting the neck area between the anterior and medial scalene muscles and the inner surface of the first rib).
 |
| Brachial plexus |
After a detailed questioning and physical assessment, we managed to treat his spine and and the nerves in that region. That cyclist was able to train without the accompanying pain and symptoms after.
Reference
Dahlstrom KA, and Oliver AB (2012). Descriptive Anatomy Of The Interscalene Triangle And The Costoclavicular Space And Their Relationship To Thoracic Outlet Syndrome: A Study of 60 Cadavers. J Manip Physiol Therapeutics. 35(5): 396-4001. DOI: 10.1016/jmpt.2012.04.017
Sunday, October 2, 2022
Coffee's Performance Enhancing Powers
Back then, I read that the caffeine in coffee was a stimulant and that it enhanced fat burning to give nuscles more energy. Another theory was that caffeine acts in the brain to make physical exertion feel easier (by blocking receptors that detect adenosine, a molecule that detects fatigue). This also helps in all out bursts of strength, prolonged endurance and cognitive effects like enhanced attention and vigilance.
Fast forward to a recent study that involved cyclists who completed time ridden to exhaustion tests at a predetermined intensity. They could sustain that intensity for around 5 minutes on 9 separate occasions. They were wired up with electrodes and other equipment before and after the rides to assess brain function, circulatory system efficiency and muscle function.
The cyclists did similar rides each time. Either 5 miligrams per kilogram body weight of caffeine was ingested an hour before the ride, or a placebo was taken. In some rides, they stopped the ride prematurely at either 50 percent or 75 percent of the time achieved in the baseline test to assess mid ride neuromuscular function.
In the final ride, the riders were given caffeine but were stopped at the exact time they had given up in the previous placebo trial to get a similar comparison of the effects of riding at a given power for a given duration with or without caffeine.
Here's a summary from the fairly complex analysis by the authors. Caffeine works! The cyclists lasted 14 percent longer (5:55 min) with caffeine compared to the placebo (5:14 min). This is equivalent to a 1 percent gain if the riders did a race or time trial.
Caffeine did help the muscles delay loss of power. Those taking the placebo at the 75 percent mark of the test had lost 40 percent of muscle power compared to less than 35 percent for those who had taken caffeine. At exhaustion those taking the placebo could generate only 60 percent less force than when they were fresh. With caffeine, the loss was 45 percent at the exact same time, pace and power.
The brain (or central nervous system) sent weaker signals to get the muscles to work when the cyclists got more tired when they ingested the placebo. With caffeine, the signals never declined, even when the cyclists reached exhaustion. Their brains were still enthusiastically getting their muscles to contract.
Caffeine also kept oxygen flowing through their arteries, as measured by a pulse oximeter attached to the cyclists' right fingers. There was only a mild decrease at exhaustion compared to a steady decline seen in those who took the placebo. The authors suggested that having more oxygen available may be one of the reasons the muscles kept working better during caffeinated rides.
This study also shows that caffeine also reduced perceived effort - just like what I read when I was 17. The pace you're holding definitely seems easier.
For those of you that are keen to try caffeine, the authors suggest 3 to 6 milligrams of caffeine per kilogram of your body weight taken an hour before your event starts. Higher doses may speed up your heart rate, not what you need during your race. Regular coffee drinkers may get a slight gain if you stop drinking coffee for a week to get that boost.
Reference
Cristina-Souza G, Santos PS, Santos-Mariano AC et al (2022). Caffeine Increases Endurance Performance Via Changes In Neural And Muscular Determinants Of Performance Fatigability. Med Sci Sports Ex. 54(9): 1591-1603. DOI: 10.1249/MSS.0000000000002944
Sunday, September 25, 2022
More Sugar More Pain?
Being in the pain business (i.e. finding the cause of patients' pain and treating it), I've always been intrigued about how we tolerate pain. Some patients can definitely tolerate pain better than others.
The article referenced below (Ye et al, 2022) definitely caught my eye. The researchers investigated the effects of high blood sugar on pain sensitivity and pain inhibition (the act of stopping or slowing down pain) in healthy adults with normal and excess body fat.
The researchers found that ingesting just 75 grams of glucose (2 standard cans of soft drink) in the overweight group of subjects caused the subjects more pain when both their feet were submerged in cold water for 1 minute.In addition, having acute hyperglycaemia (high blood sugar levels) also suppressed resting heart rate variablity (HRV) in the group with excess fat mass. *HRV is where the amount of time between your heart beats fluctates slightly.These fluctuations can indicated current or future health problems like heart conditions or anxiety and depression.
Regardless of blood sugar levels, the group with excess fat mass could not tolerate the pain from a pin prick after cold water immersion. This group also reported higher pain levels during a 5-minute period of blood flow occlusion.
In addition to the effects of high blood sugar on pain sensitivity and pain inhibition, effects on HRV and reactive hyperaemia (increase of blood flow) after arterial occlusion were also investigated. Both high blood sugar and excess body fat affected HRV and reactive hyperaemia only in people with extra fat mass.
Interpreted together, the researchers concluded that high blood sugar levels affected pain processing levels and autonomic function, especially in people with excess body fat mass.
So, if you are overweight and consume more than 75 grams of sugar (2 standard cans of soft drinks) you will more likely feel more pain compared to someone who is not overweight.
The authors added that since both hyperglycaemia (high blood sugar levels) and being overweight are risk factors for diabetes, further research should be done on whether and how these sources of pain affects people with diabetes.
Reference
Ye D, Fairchild TJ, Vo L et al (2022). High Blood Glucose And Excess Body Fat Enhance Pain Sensitivity And Weaken Pain Inhibition In Healthy Adults: A Single-blind And Cross-over Randomised Controlled Trial. J of Pain. In Press, published 16 Sep 2022. DOI: 10.1016/j.pain.2022.09.006
*HRV responds uniquely for everyone. As a rule of thumb, values under 50 ms are unhealthy, 50-100 ms signal compromised health and readings above 100 ms are healthy.