|
| Picture by Oyvind Solstad from Flickr |
Don't we all love shoes that are comfortable? Especially when it comes to our running shoes. As runners, we all love that ahhhh sensation of our first steps in an exceptionally soft and comfy shoe. I couldn't believe how soft an Adidas NMD (not really running shoe though) felt when I first slipped it on. A more comfortable (or cushioned) shoe is usually preferred by new runners or for runners who are prone to injury and want extra protection and support.
The shoe companies know that subjective comfort is an essential factor in sport shoe development since this definitely helps them sell shoes. This comfort paradigm is based on an assumption that perceived comfort will lead to a path of least resistance (while running) and potentially reduce injury and improve running economy. (Luo et al 2009; Mundermann et al, 2001).
One study showed reduced oxygen consumption levels during running at submaximal speed while running in shoes that were rated subjectively as most comfortable (Luo et al, 2009). This may support the fact that running economy improves due to reduction of muscle activation (which decreases oxygen consumption or metabolic demand).
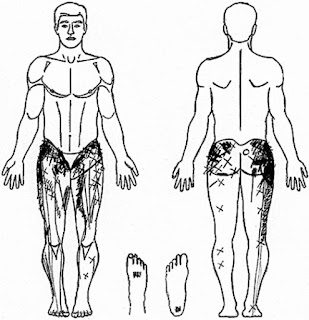
Another study on military personnel showed some evidence supporting the use of comfortable shoe inserts (or orthotics) reduced injury rates of the foot, ankle, hip, knee and lower back compared to a control group. However, two studies are not credible enough to know what actually helps and what are the mechanisms of reduction in oxygen consumption and preventing injuries. (Both studies count Professor of Biomechanics Benno Nigg, known for his work of running shoes as one of the authors).
In this latest paper I read, the authors aimed to investigate how shoes of differing comfort affects differences in oxygen demand along with potential mechanisms associated with injury risk.
Fifteen male runners who ran at least 20 km per week with treadmill experience were recruited for the study. Testing includes an incremental lactate threshold test, a comfort assessment and treadmill running trials for biomechanical and physiological assessments.
The researchers did not find any decrease in oxygen consumption in the most preferred shoe. Potential biomechanical contributors to changes in oxygen consumption (or metabolic demand) showed some differences in stride rate between the most preferred and least preferred shoe. Personally, it was interesting for me to note that stride frequency was actually lower in the most preferred (or comfortable) shoe compared to the least preferred (or least comfortable).
Based on the findings of this study, previous suggestions (derived from two other studies) regarding positive effects of enhanced footwear comfort during running cannot be supported. Neither on running economy nor on preventing injuries.
Should we then choose our running shoes based on comfort alone? This study suggest maybe not since the most comfortable shoes were not better or worse off with regards to oxygen consumption and not enough data to show any real change on injury risk.
Comfort is just one of many factors when we choose running shoes (compared to the more common foot type option like overpronators, supinators etc). Of course I definitely would not suggest running in shoes that are uncomfortable.
I'm also feeling appalled that only 15 male runners (and no female runners) were selected for the study. Remember I write previously how difficult it is to recruit runners to participate in a running research.
Athletes will want shoes that give them absolute efficiency that helps that run faster while your average runner would want the least discomfort while running to get fit.
Of course there are some runners that will choose based on colour! *facepalm*
References
Lindorfer J, Kroll J and Schwameder H (2019). Does Enhanced Footwear Comfort Affect Oxygen And Running Biomechanics? Eur J Sport Sci. 20(4): 468-476. DOI : 10.1080/17461391.2019.164028
Luo, G, Stergiou P et al (2009). Improved Footwear Comfort Reduces Oxygen Consumption During Running. Footwear Sci. 1(1): 25-29. DOI: 10.1080/194242809002993001
Mundermann A, Stefanyshyn DJ and Nigg BM et al (2001). Relationship Between Footwear Comfort of Shoe Inserts and Anthropometric And Sensory Factors. Med Sci Sport Ex. 33(11): 1939-1945. DOI: 10.1097/00005768-200111000-00021.
Notes on the shoes in this study provided by Adidas
Five different shoes based on criteria previously reported in another study (Luo et al, 2009) were provided for this study. The shoe conditions showed variations in total mass (80 grams), heel lift (3.7mm), forefoot cushioning, rearfoot cushioning forefoot bending and rearfoot bending. The shoes in this study includes a standard neutral running shoe, shoes equipped with non standardized features like carbon fiber plates for increased longitudinal bending stiffness, exaggerated arch support and a cross training shoe.
One interesting point was that the researchers glued lead to the heel counters of the shoes that were lighter (since shoe mass influences oxygen consumption by about 1% per 100 grams of additional mass).