|
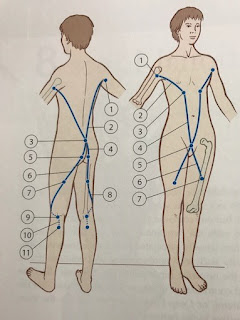
| Kindly drawn by my older son |
The cause of OCD is unknown. It is suggested that reduced blood flow to the bone may occur from repetitive trauma like excessive running and jumping. Or small, multiple episodes of minor unknown injury that damage the bone over time. Some studies suggest that there may be a genetic component involved too.
OCD occurs most frequently in children and adolescents, most commonly in the knee, but can also occur in the elbow and ankle.
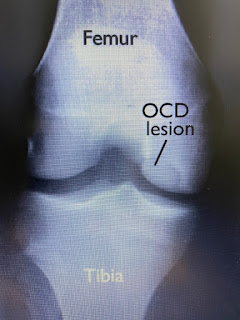
Doctors stage OCD according to how big the bone fragment is, whether the bone fragment is totally or partially separated or whether it stays in place. If that loosened piece of bone is not detached, then there may be few or no symptoms. For younger children whose bones are still growing and developing, there is a chance that it can heal.
So it was a total surprise to me when my adult patient was diagnosed with OCD 2 days ago.
She was in the process of sitting down on her sofa and slightly twisted her knee. She could not extend or bend her knee fully nor put weight on her foot after that. She went to the hospital and was told it might be a meniscus tear and may need surgery. The surgeon suggested an MRI to confirm his hypothesis.
Hence, when the MRI results came out it was a big surprise that there was a bone fragment dislodged. That's the reason why she could not straighten or bend her knee fully.
The only incident my patient could think of was during gymnastics, when she was 12, that her knee started to hurt (possibly from the impact of repeated running and landing). Her knee would 'lock' occasionally for a few days at a time. It gradually resolved and she would occasionally have some knee pain on that same left knee while she competed in triathlons. Otherwise, there was no other clue that she would have OCD.
Now my patient has to decide how she would like to proceed to get the bone fragment out after discussion with her surgeon.
Reference
Kocher MS, Tucker R, Ganley TJ et al (2006). Management Of Osteochondritis Dissecans Of The Knee: Current Concepts Review. AJSM. 34(7): 1181-1191. DOI: 10.177/0363546506290127.
 |
| Picture from RadioGraphics |