|
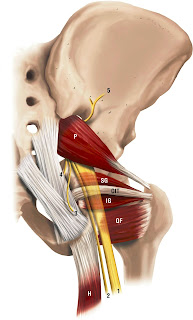
| Right Piriformis muscle and the sciatic nerve |
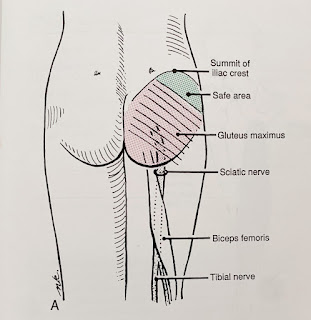
The sciatic nerve can get encroached or irritated by the piriformis and adjacent structures in that deep gluteal space which may result in pain at the area of irritation or along the path of the sciatic nerve - this is true sciatica pain.
After assessing my patient, there was no pain nor tenderness in her piriformis. Instead, her obturator internus reproduced her buttock pain.Coincidently, I was fortunate to have read a recently published article exploring the relationship of the sciatic nerve and the deep hip external rotator muscles in the deep gluteal space (Balius et al 2022).
The authors recruited 58 healthy volunteers, 30 males and 28 females with an average age of 20.4 years plus or minus 7 years using real time ultrasound to quantify nerve action.
The sciatic nerve was found to be compressed (and moved forward and laterally) during passive hip internal rotation and isometric external rotation contraction (obturator internus and gemelli muscles working). Not the piriformis muscle, which the authors wrote were often over diagnosed.
During passive hip external rotation and isometric contraction of internal hip rotators, the sciatic nerve moved back into place and medially.
The obturator internal-gemellus syndrome may be a more accurate term than piriformis syndrome for my patient.
Interestingly, the same lead author, Balius and colleagues, published an earlier article in 2018 where they studied 6 fresh cadavers and 31 healthy volunteers. This study revealed the presence of connective tissue (or fascia) attaching the sciatic nerve to the obturator internus-gemellus tendons. The sciatic nerve was also affected similarly in the cadavers and subjects during passive hip internal rotation.
This newer study (Balius et al, 2022) provides further evidence that stretch or contraction of the obturator internus-gemellei complex will create some compression of the sciatic nerve at this level in the deep gluteal space. Definitely worth considering for those with buttock pain and sciatica.
The next time you have buttock pain or sciatica and the health practitioner treating you tells you that you have piriformis syndrome you may suggest it's not always the piriformis ;)
Reference
Balius R, Pujol M, Perez-Cuenca D et al (2022). Sciatic Nerve Movements In the Deep Gluteal Space During Hip Rotations Manuevers. Clinical Anatomy. 35(4): 482-491. DOI: 10.1002/ca.23828
Balius R, Sussin A, Morros C et al (2018). Gamellei-obturator Complex In the Deep Gluteal Space: An Anatomic And Dynamic Study. Skeletal Radiol. 47: 763-770. DOI: 10.1007/s00256-017-2831-2